~Written by Victoria Stanford (Contact: vstanford@hotmail.co.uk)
Tents below a motorway pass, Piraeus Port, Greece. Photo credit: Victoria Stanford
The number of refugees arriving in Europe continues to rise, despite the EU-Turkey deal struck in March 2016 aimed at halting the numbers of new arrivals. This deal represented one of the first consensual decisions made by the 28 member states of how to respond to the unprecedented refugee crisis in Europe seen over recent years. However, across Europe there remains an overwhelming lack of political effectiveness, or indeed will, to co-ordinate the care of those arriving on the continent. Supranational institutions, European governance bodies, NGOs and humanitarian partners have scrambled in varying degrees of commitment to offer their services to refugees and the impression for many is that they are not achieving enough, quickly enough. But how have the various actors responded to the health needs of the refugees, and who is held accountable for this most basic human necessity?
Arrival versus Settlement
There is a significant difference between the immediate and long-term healthcare needs seen among refugee populations. This protracted crisis must be able to respond to both the immediate and often-life saving measures needed on Greek islands where refugees are still arriving by boat, and the long-term needs of refugees who have settled in host countries, in many cases for months or even years. Understanding this transition between the emergency and post-emergency phase, is essential for planning an effective healthcare response. The needs of those new arrivals mostly consists of sanitation, nutrition, shelter and basic safety provision, whilst those further along the asylum process must be integrated into long-term health systems that provide them with more complex and comprehensive services such as chronic disease management.
As it stands, the initial needs of refugees arriving to European shores are often provided by humanitarian agencies who are equipped to launch an emergency response, and gradually they hand over this responsibility to the local health care structures. An excellent example of this was seen in Bulgaria when Doctors without Borders provided medical care to over 1500 refugees, allowing the national authorities who have now taken over healthcare service provision in this area, to build capacity and prepare (1). In many places this handover scenario has not been achieved so clearly and in fact often it is best for organisations and local partners to share the healthcare responsibilities. For example in Piraeus port in Athens (now dissolved), NGOs such as Praxis and the Red Cross were stationed within the camp itself and acted as primary care providers to the population on the ground, referring patients who required more specialised care on to state-run and funded hospitals or clinics in Athens. A similar system is currently established between the residents of the Jungle camp in Calais and the PASS clinic (Permanence d'Accès aux Soins de Santé)-provided by the government for refugees and others without social security insurance in France. However the extent to which this collaborative effort is effective depends much on the nature of the healthcare needs required; patients with mental health issues requiring long-term psychological treatment or those with post-surgery rehabilitation needs are often prematurely discharged or simply not offered longstanding care. Logistical difficulties are also often neglected as many appointments and consultations are arranged in neighbouring cities and patients are required to arrange their own transport which for many is an impossibility. Achieving adequate provision and access in healthcare for refugees is complex and is largely dependent on context, their status in the asylum process and capacities of local health organisations.
The ‘Unofficial’ Refugee
Much complexity has been added to this crisis by the lack of clarity in defining those who are arriving in Europe- undocumented migrants, labour migrants, refugees and asylum seekers are terms often confused and used interchangeably and this has an impact on how these people can interact with official services. As refugees and others spread across Europe, the way in which they settle varies dramatically-there are families living in air-conditioned containers in official UN-led refugee camps, whilst others squat in abandoned buildings in the suburbs of Athens. This undoubtedly leads to much heterogeneity in terms of both their access to and quality of healthcare. Much of the healthcare that refugees living in official camps receive is provided by large, international NGOs such as Doctors without Borders (MSF) or the Red Cross. These organisations provide high-standard medical and nursing care, including psychological support in many cases, and also organise public health services such as child immunisations. As priority for official camp accommodation is usually given to families with children or vulnerable people with either chronic diseases or disabilities, providing comprehensive healthcare services to these populations is even more imperative. What this means however, is that resources are stretched thin and those refugees who are either in transit or living in unofficial areas often receive a lower quality or even a complete lack of healthcare.
The legal status of a refugee can also be a barrier to seeking healthcare, particularly in the few chaotic months after arrival in Europe. Many do not fully understand their legal rights or how to access healthcare in host countries; this is particularly problematic for those who are not settled immediately into official camps, instead attempting to cross international borders or avoid registration for fear of the barriers this may pose to freedom of movement (2). This means many do not receive their healthcare entitlements and depend on the ad-hoc and inconsistent presence of healthcare-providing groups often from outside any official aid delivery process.
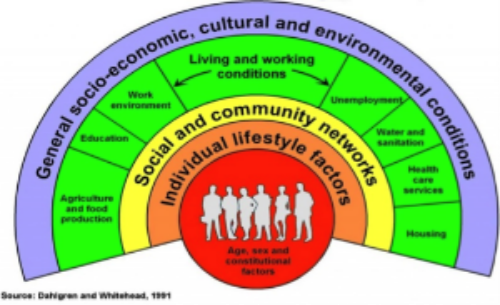
The ‘unofficial’ refugee population is in fact where the grassroots organisations have trumped more established humanitarian groups. Countless groups have been set up in recent years by concerned citizens across Europe and have provided the in-the-field manpower that many official partners have failed to do. Groups such as Drop in the Ocean, Care 4 Calais, Help Refugees and many others have integrated into the ‘official’ aid delivery system and have in many cases outpaced those organisations who are often restricted by mandates or internal bureaucracy. These groups offer assistance that is not always recorded on health surveillance statistics or official reports but in fact they are in many cases acting as primary carers. As healthcare itself is not the only way of keeping refugees healthy, these groups who attend to other needs such as shelter and food provision, hygiene, childcare and education may actually be having a significant impact on the refugee population’s health (3).
What about the Supranationals?
Red Cross Measles Vaccination Campaign, Scaramangas Camp, Athens. Photo credit: Victoria Stanford
Under the 1951 Refugee Convention, refugees should enjoy access to health services equivalent to the host population, and institutions such as the World Health Organisation (WHO) and the Office of the United Nations High Commissioner for Refugees (UNHCR) are tasked with upholding these rights under the UN Charter (4). It is increasingly clear that Europe is struggling to deal with the crisis and the UN has put pressure on European governance bodies to establish a comprehensive, mutually-agreed response plan to address the health needs of the refugee populations. This has achieved some success particularly in communicable disease control with large-scale vaccination programmes used in camps and non-camp settings alike (5) (see photo).
However, the long-term nature of this crisis will require more of a focus on capacity-building of existing healthcare structures in host countries. For this reason, the WHO has performed a number of Assessment missions in countries receiving the most footfall of refugee movement including Cyprus, Greece, Italy and others, providing countries with context-specific information and guidance on responding to the health needs of refugees either temporarily or permanently settling in these countries (6). These analyses of the current preparedness of national health structures have helped to pinpoint where increased funding or skills are needed to boost local response; the European Commission have subsequently invested over 5 million euros on projects with the aim of “supporting member states under particular migratory pressure in their response to health-related challenges” (7). Crucially, these projects integrate NGOs with national structures, bridging the gap between short and long-term response, and focus on fostering comprehensive access to all aspects of the health system, not only emergency care. One of these projects also places a particular focus on the health needs of pregnant women, unaccompanied minors and young children, highlighting a concern for the most vulnerable populations in this crisis (7). However, whilst these projects are theoretical problem-solvers, there is a gap between plan and action. Many projects will take years to see results and whilst they do, countries such as Greece are reliant on existing health care systems, which have been struggling for years to cope with both the steady influx of refugees over many years and domestic austerity policies (8).
The bottom line is that funded and elected institutions such as the UN are mandated to protect the rights of refugees and these include access to healthcare. This situation sees the heavily bureaucratised system overloaded and rendered flimsy by the sheer volume of refugees depending on it, not only in Europe. This has meant that other humanitarian partners and grassroots movements have stepped in and provided invaluable assistance on the ground. The provision of healthcare to refugees in Europe largely depends on capacity and it is clear that there must be far-reaching plans made to build on both national and international health system structures. Whether these plans will materialise into effective action that both prevents ill health and treats disease remains to be seen as the crisis, without long-term solutions, inevitably continues.
References:
(1) MSF (2016) Bulgaria: providing healthcare to Syrian refugees [Online] Available at: http://www.msf.org.uk/article/bulgaria-providing-healthcare-syrian-refugees [Accessed August 2016)
(2) Global Health Watch (2015) Migrants and asylum seekers; the healthcare sector, London, Page 63.
(3) Kuepper, M (2016) Does Germany need to rethink its policies on refugees? Researchgate.net [Online] Available at: https://www.researchgate.net/blog/post/does-germany-need-to-rethink-its-policies-on-healthcare-for-refugees [Accessed August 2016]
(4) UNHCR; Health (2016) [Online] Available at: http://www.unhcr.org/uk/health.html [Accessed August 2016]
(5) UN News Centre (2015) UN seeks common European strategy on healthcare for refugee and migrant influx [Online] Available at: http://www.un.org/apps/news/story.asp?NewsID=52630#.V7DT6_krK01 [Accessed August 2016]
(6) WHO (2015) Stepping up action on migrant and refugee health [Online] Available at: http://www.euro.who.int/en/countries/greece/news/news/2015/06/stepping-up-action-on-migrant-and-refugee-health [Accessed August 2016]
(7) European Commission Health Programme (2015) Health projects to support member states, Geneva.
(8) Chrisafis, A (2015) Greek debt crisis: of all the damage, healthcare has been hit the worst, The Guardian, 9 July 2015 [Online] Available at: https://www.theguardian.com/world/2015/jul/09/greek-debt-crisis-damage-healthcare-hospital-austerity [Accessed August 2016]